Lupine Publishers Anesthesia Pain Medicine Journal
Thursday, November 24, 2022
Happy Thanksgiving 2022!!
Saturday, November 12, 2022
Anesthesia for Transurethral Resection of Bladder Tumors in Patients with Neuropathy Caused by Balloon- Occluded Arterial Infusion Treatment: A Retrospective, Observational Study
Background: A novel bladder preservation therapy has been developed for patients with muscle-invasive bladder cancer called the Osaka Medical College (OMC) regimen. This regimen comprises balloon-occluded arterial infusion (BOAI) of an anticancer agent and with or without concurrent hemodialysis. Anticancer agents, such as cisplatin, can cause neurotoxicity, leading to peripheral neuropathy. This study aimed to investigate the occurrence of neuropathy after BOAI followed by a second transurethral resection of a bladder tumor (TURBT). We also aimed to investigate the effects of general and spinal anesthesia on neuropathy.
Methods: We performed a retrospective, observational study on 57 patients (49 men, 8 women, median age: 65 years) with bladder cancer who underwent a second TURBT after BOAI. TURBT was initially performed for diagnosis and then patients received the OMC regimen at 4-5 weeks after this first TURBT. Patients had general or spinal anesthesia for TURBT. For BOAI, an intra-arterial catheter with two occlusion balloons was used and inserted into the posterior trunk of the internal iliac artery. Cisplatin was infused through this catheter over 1 hour. Hemodialysis was simultaneously performed in patients (n=16) with a creatinine level >1.5mg/ dl. Radiation therapy was then performed in the pelvis. Patients underwent a second TURBT at 6 weeks.
Results: Seven of 57 patients had neuropathy. Symptoms caused by BOAI in the lower extremities were pain, numbness, and tingling. Although none of the treatments for neuropathy were particularly effective, the combination of tramadol and acetaminophen reduced tingling in one patient. No patients had adverse events of grade 3 or 4. Two patients who had abnormal sensation before the second TURBT underwent general anesthesia to avoid any further deterioration.
Conclusion: This study showed that neuropathy occurs after BOAI of cisplatin for bladder cancer. Although there was no deterioration in sensation of the lower extremities in patients who had a second TURBT under general or spinal anesthesia, further deterioration in sensation is possible. Therefore, spinal anesthesia should be avoided in patients who have neuropathy due to BOAI. Trial Registration: This study was registered in the Japanese Official Clinical Trial Registry (trial registration number: JMAIIA00171) and the registration date was 13 March 2014.
Read more about this article: https://lupinepublishers.com/anesthesia-pain-medicine-journal/fulltext/anesthesia-for-transurethral-resection-of-bladder-tumors-in-patients-with-neuropathy-caused-by-balloon-occluded-arterial-infusion-treatment.ID.000104.php
Read more Lupine Publishers Google Scholar Articles: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=fEgaZz4AAAAJ&citation_for_view=fEgaZz4AAAAJ:LkGwnXOMwfcC
Wednesday, December 23, 2020
Wishing you a Magical and Blissful Holiday!
Have a Merry Christmas and a Happy New year! I hope Santa is good to you this year because you only deserve the best. Merry Christmas from our family to yours. Take nothing for granted and be thankful that you have such great family and friends to spend this joyous season with.
Wishing you a delightful Christmas and a very Happy New year in Advance.
Friday, March 6, 2020
Is There A Neck-Shoulder Syndrome?| Lupine Publishers
Lupine Publishers| Anaesthesia and Pain Medicine Journal
Abstract
Keywords: Neck and shoulder pain; Neck-shoulder syndrome; Pain treatment; Differential diagnosis of neck and shoulder pain
Introduction
Discussion
Primary neck pathology with referred pain to the shoulder
An isolated C5 and/or C6 radiculopathy without shoulder pathology could certainly present with neck and shoulder pain due to C5 and C6 dermatomal symptoms corresponding to the shoulder region. C5 or C6 myotomal pain can cause pain in the deltoid, scapula and biceps, and can mimic shoulder pathology [8,9]. This scenario is typically straightforward as the physical examination will be absent of shoulder impingement signs. Classically, cervical radiculopathy examination can demonstrate positive cervical root impingement signs (Spurling’s maneuver), myotomal weakness, dermatomal sensory abnormalities and blunted reflexes in a specific root distribution. Several neuropathies involving brachial plexus and its proximal branches will also refer pain to neck and shoulder simultaneously.Primary shoulder pathology with referred pain to the neck
Primary shoulder pathology should not directly lead to neck pathology, and such cases are not well described in the literature. Nevertheless, patients with shoulder pathology may develop pain and tightness in the trapezius muscle on the ipsilateral side and referred pain in the cervical area. Restricted motion at the glenohumeral joint may also lead to overuse and pain in the scapulothoracic musculature. A general concern in musculoskeletal medicine is that symptomatic pathology in a joint may refer pain to a joint below and/or above.Primary neck and primary shoulder pathology
Degenerative arthritis can affect multiple joints. Thus, many patients may have both glenohumeral arthritis and cervical spondylosis. The radiographic incidence of glenohumeral arthritis is reported as 32.8% in people over 60 years of age [10]. Radiographic evidence of cervical spondylosis is present in 50% of people over 50 years of age and 75% of individuals over 65 years of age [11]. As both conditions are common, both can present as “pain generators.”Primary neck pathology resulting in secondary shoulder pathology
Primary neck pathology resulting in secondary shoulder pathology is mechanically plausible although not proven. For instance, C5 and/or C6 cervical radiculopathy can result in rotator cuff, deltoid, biceps and scapular muscle weakness as these nerve roots innervate the shoulder girdle musculature. This could produce muscle imbalance and poor shoulder/scapular mechanics. A patient may present with features of both cervical radiculopathy and shoulder impingement syndrome in this scenario. In clinical practice, it is not uncommon to see a patient with chronic neck pain presenting with insidious onset of shoulder pain later in the course. Authors are proposing this unique presentation be referred to as “neck-shoulder syndrome.” Although most clinicians would treat this as separate neck and shoulder pain, they may be related diagnoses.Literature Search
Presentation
Location: Patients with primary neck pathology can experience pain extending beyond the neck based on the etiology. Disorders that affect the lower cervical nerve roots will often result in pain distal to the shoulder which can be characterized by radiation into the arm in a clear dermatomal or myotomal distribution [12]. In addition, Dwyer et al described reproducible pain patterns that can refer into the shoulder, trapezius and occiput from cervical zygapophyseal joint pathology [13-15]. Pain from a primary shoulder problem can also refer pain to the neck, periscapular region and distally into the arm although not typically extending below the elbow [16]. Associated paresthesias are not classically associated with a primary shoulder problem.
Onset: Onset of symptoms is also a key component of the history. Degenerative cervical pathology can have insidious onset although acute disc herniations can have a sudden onset that may be precipitated by trauma. Whiplash injuries are known to precipitate neck pain which can be of myofascial and/or cervical facet in origin. Shoulder disorders can also be of insidious (overuse injuries) or acute onset (trauma). Sudden onset of shoulder pain with restricted motion can be associated with acute calcific tendinitis or adhesive capsulitis. Neuralgic amyotrophy (Parsonage Turner syndrome/ brachial neuritis) has a unique presentation where patients usually experience severe, acute pain following exercise, recent illness, immunization, surgery or trauma [17]. As the initial severe pain starts to resolve, neurological deficits will become apparent, which is in contrast to most presentations of cervical radiculopathy where pain will continue with associated neurological symptoms. Onset of symptoms plays a key role in proper identification of proposed “neck-shoulder syndrome.” Development of shoulder pain (especially in the absence of injury) after onset of neck/radicular pain can be considered primary neck pathology with secondary shoulder pathology and can be referred to as “neck-shoulder syndrome.” Shoulder pain in this scenario is likely secondary to rotator cuff and periscapular muscle weakness/imbalance caused by C5 and/or C6 cervical radiculopathy. This clinical scenario is not well studied in the literature, hence prevalence and incidence is not known. Among patients with cervical radiculopathy, studies report a frequency of C5 nerve root involvement at 5-10%, C6 at 20-25%, and C7 at 45-60% [12,18].
Exacerbating factors: Pain with overhead arm movements generally suggests primary shoulder pathology. However same pattern can also be present in peripheral neuropathies like thoracic outlet syndrome and spinal accessory, suprascapular, or axillary neuropathy. Shoulder pain with side lying on the affected upper limb tends to be associated with shoulder impingement and acromioclavicular joint arthropathy.
Features of systemic diseases: In patients who present with neck and shoulder pain in the absence of trauma, the history will need to include an assessment for widespread involvement that may suggest systemic disease processes like fibromyalgia, polymyalgia rheumatica, myofascial pain syndrome and myopathy.
Red flags: The history should also include an evaluation for findings to suggest a disease process that requires more urgent evaluation. Red-flag symptoms to assess for include gait imbalance, hand clumsiness, bowel/bladder dysfunction (cervical myelopathy), pain after high impact trauma (fractures), unintentional weight loss (Pancoast tumor), chest pain (cardiac ischemia), blurry vision, nausea/vomiting and vertigo (vertebral artery dissection/ insufficiency).
Physical Examination
Provocative Testing
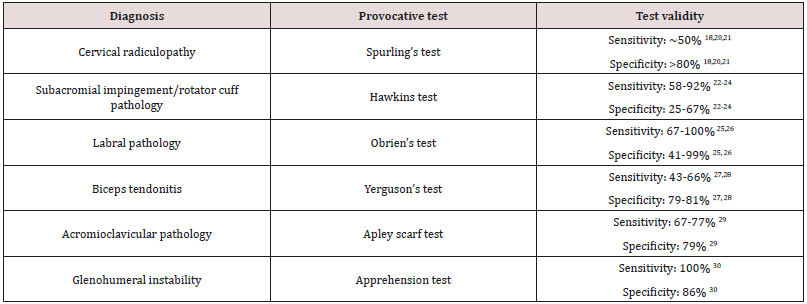
Provocative testing can assist in the diagnosis of cervical and shoulder disorders [9, 19]. Among them, provocative tests for shoulder impingement may help distinguish primary versus secondary shoulder pathology in proposed “neck-shoulder syndrome”(Table 1) [18-30].In patients with neck and shoulder pain, one test by itself may not have enough sensitivity and specificity to make a diagnosis and most physical exam maneuvers are not pathognomonic. A combination of multiple exam components and a thorough history are necessary to accurately identify the etiology of symptoms.
Diagnostic Testing
Treatment
Conclusion
Acknowledgements
For more Lupine Publishers Open Access Journals Please visit our
website:
For more Global
Journal of Anesthesia & Pain Medicine articles Please Click Here:
To Know More About Open Access Publishers Click on Lupine
Publishers: https://lupinepublishers.com/
Read More Lupine Publishers Anesthesia Journal Articles : https://lupine-publishers-anesthesia.blogspot.com/
Read More Lupine Publishers blogger Articles : https://lupinepublishers.blogspot.com
Read More Lupine Publishers blogger Articles : https://lupinepublishers.blogspot.com
Friday, January 24, 2020
Lupine Publishers: Lupine Publishers: Lupine Publishers | Hamstring I...
Monday, January 13, 2020
Lupine Publishers: Lupine Publishers | A Mini Review- Investigation a...
Friday, January 10, 2020
Lupine Publishers: Lupine Publishers | A Mini Review- Investigation a...
Happy Thanksgiving 2022!!
Thanksgiving is a joyous invitation to shower the world with love and gratitude. Forever on Thanksgiving the heart will find the pathway h...

-
Thanksgiving is a joyous invitation to shower the world with love and gratitude. Forever on Thanksgiving the heart will find the pathway h...
-
Abstract: Background : A novel bladder preservation therapy has been developed for patients with muscle-invasive bladder cancer called th...
-
Lupine Publishers: Lupine Publishers: Lupine Publishers | Hamstring I... : Lupine Publishers: Lupine Publishers | Hamstring Injuries in Taek...